causes or reason for heart attack at an early age
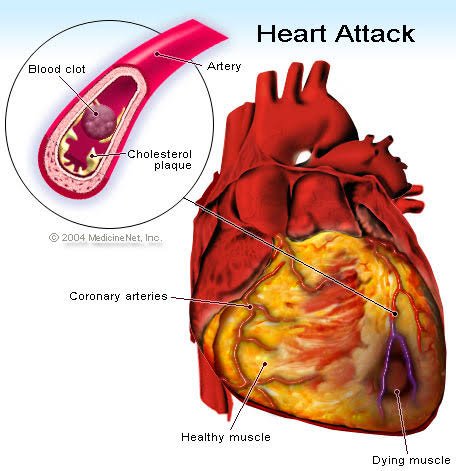
Myocardial infarction (MI), commonly known as a heart attack, can be caused by several factors, including:
1. Stress
In addition to interventional procedures, medications are often administered to manage acute MI. These may include:
- Blood thinners
- Antiplatelet drugs
- Pain and stress relievers
- Medications designed to dissolve blood clots
- Medications to control blood pressure, among others.
Preventing acute Attacks
Taking proactive steps can significantly reduce the risk of myocardial infarction (MI) and promote long-term health. Here are some key strategies to help prevent heart attacks, especially at a young age:
- Adopt a balanced diet that includes plenty of fiber-rich foods.
- Limit your intake of sodium and salt.
- Minimize consumption of packaged and processed foods.
- Regularly monitor your blood sugar, blood pressure, and cholesterol levels.
- Quit smoking and refrain from having secondhand smoke.
- Maintain an active lifestyle through regular exercise and physical activity.
Also Read: Meditation For Positive Life
The increasing incidence of acute MI among young adults as serves as a warning sign that demands attention. However, by staying vigilant, practicing self-care, and embracing a healthy lifestyle, you can effectively lower your risk of this life-threatening condition.
Disclaimer
The information provided herein is for informational purposes only and should not be considered as medical advice. It is not intended to diagnose, treat, cure, or prevent any disease or condition. Always consult with a qualified healthcare professional regarding any medical concerns or questions you may have. Reliance on any information provided in this communication is solely at your own risk. The author and publisher disclaim any liability for any adverse effects resulting directly or indirectly from using or applying the information contained herein.




